Key Takeaways
Bipolar disorder is a mental health condition with moods that shift between depressive and manic/hypomanic.
Depressive episodes involve a low, sad, or hopeless mood and a loss of interest in activities you used to enjoy. Manic and hypomanic episodes are characterized by energy, feelings of euphoria, and less need for sleep.
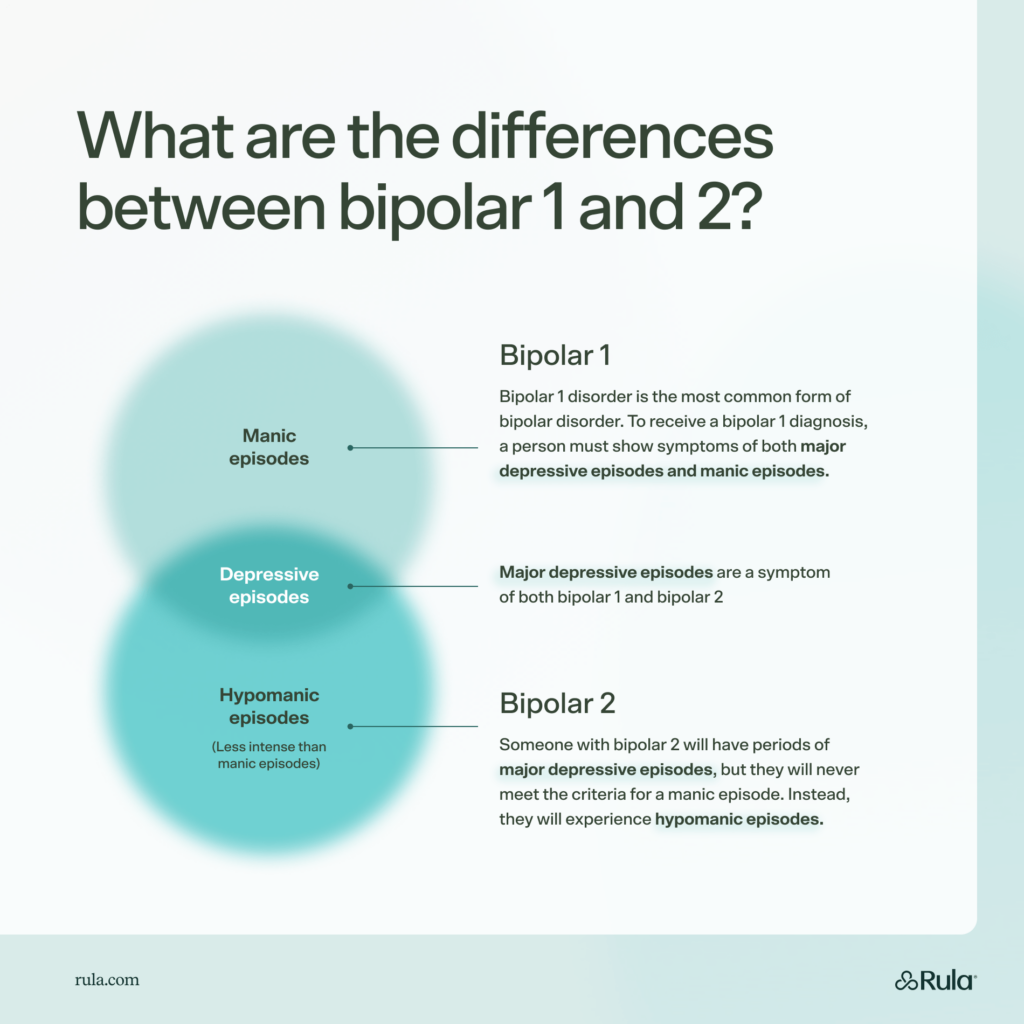
With bipolar disorder 1, people experience both major depressive episodes and manic episodes. In bipolar 2 disorder, people have depressive episodes and hypomanic episodes (which are less intense than manic episodes).
Bipolar disorder is not only one condition. Instead, it’s a collection of related diagnoses that all involve shifts between low- and high-mood episodes. Though different and distinct, all forms of bipolar disorder can be difficult for both the person with the condition and the people who care about them.
Treatment options for bipolar disorder are available, and knowing how to recognize the symptoms is the first step toward getting effective care.
What is bipolar 1?
Bipolar 1 disorder is the most common form of bipolar disorder. To receive a bipolar 1 diagnosis, a person must show symptoms of both major depressive episodes and manic episodes.
Depressive episodes
Major depressive episodes are periods where a person has:
Depressed or irritable mood
Less interest in activities
Unintentional weight loss or gain
A need for significantly more or less sleep
A feeling of being sped up or slowed down
Low energy and fatigue
Feelings of worthlessness or guilt
Decreased ability to think clearly
Thoughts of death and dying
To be considered a depressive episode, a person needs to have at least five of these symptoms during the same two-week period.
Manic episodes
During a separate one-week period, a person with bipolar 1 will experience symptoms of a manic episode. Manic episodes involve a mood that is highly elevated or irritable. They will also have a series of related symptoms that may include:
High self-esteem and ideas of importance
Lower need for sleep
Being very talkative
Moving from topic to topic very quickly
High distractibility
Being driven to complete a goal or appearing restless
Being very engaged in risky activities or behaviors
With manic episodes, this period of boosted mood and high energy levels will last for at least one week. The person will show three or more of the above symptoms. The person may feel driven to complete grand goals without a good plan. They may move fast, talk fast, and require limited food and sleep.
It’s helpful to note, though, that with bipolar disorder, people may experience long periods of typical functioning between mood episodes. Other people may cycle more quickly from episode to episode.
What is bipolar 2?
Bipolar 2 disorder shares many of the same symptoms as bipolar 1. Someone with bipolar 2 will have periods of major depressive episodes, but they will never meet the criteria for a manic episode. Instead, they will experience hypomanic episodes.
Hypomanic episodes
During a hypomanic episode, the person will report and show the same types of symptoms seen in manic episodes, but they will be shorter and generally less intense. While manic episodes last for at least a week, hypomanic episodes only need to last for four days.
So someone with depressive and manic episodes will have bipolar 1 disorder, and someone with depressive and hypomanic episodes will receive a bipolar 2 disorder diagnosis. Other conditions can produce similar symptoms, but subtle differences separate them from bipolar disorder.
Five key differences between bipolar 1 and bipolar 2 disorder
It may seem like a slight technical difference that separates bipolar 1 from bipolar 2, but these conditions are noticeably distinct.
Here are a few key differences between bipolar 1 and bipolar 2:
Mania vs. hypomania: People with bipolar 1 disorder experience periods of mania, also known as manic episodes. People with bipolar 2 disorder experience hypomania, which is a shorter episode of elevated mood.
Risky behavior: The impact of a longer manic episode is usually riskier and more detrimental than a hypomanic episode. For example, during manic episodes, a person is more likely to injure themselves or endanger others. Even with hypomanic episodes, a person’s symptoms can affect their relationships or job. But they will never experience the full effects of mania.
Psychotic symptoms: People with bipolar 1 may also experience psychotic symptoms, like hallucinations or delusional thinking. They are also more likely to need to be hospitalized than people with bipolar 2.
Onset time: Bipolar 2 disorder tends to start slightly later in life than bipolar I, but symptoms of both conditions often start when people are in their mid-20s.
Rates of occurrence: The first type is also much more common, with about twice as many people having bipolar 1 disorder compared to bipolar 2.
Treatment options for bipolar 1 and 2
The treatment options for bipolar 1 and bipolar 2 are very similar. A combination of medication management and therapy is a first-choice treatment for both types of bipolar disorder.
Medication
Medications can help shift moods away from a depressive or manic/hypomanic state and toward a place of balance. And therapy can help people learn to notice their changing moods. Then, they can learn to modify their thoughts, feelings, and behaviors to stabilize their symptoms.
Therapy
Many types of therapy can help treat bipolar disorder. Some therapy options for bipolar 1 and 2 include:
Cognitive behavioral therapy (CBT): CBT helps people investigate their thoughts, feelings, and behaviors while teaching them healthy coping skills.
Family-focused treatment (FFT): Since bipolar disorder can affect both the person with the condition and their loved ones, FFT involves family members. This approach helps the person with bipolar disorder and their family improve their communication skills, knowledge, and problem-solving skills.
Interpersonal and social rhythm therapy (IPSRT): IPSRT helps people with bipolar disorder learn to track and manage their sleep/wake cycles and social rhythms to better manage their symptoms.
Lifestyle changes
Lifestyle changes can also help people minimize the impact of their bipolar disorder symptoms. Some helpful lifestyle choices include:
Paying attention to a healthy diet
Getting regular exercise
Maintaining good sleep hygiene
Spending time with loved ones
Finding fulfilling work or hobbies
Joining a bipolar disorder support group
A combination of treatment options is usually best for people with bipolar disorder. And you’re more likely to see progress if you stay consistent with your treatment.
Can you have bipolar 1 and 2, and can you switch between them?
No, you can’t have both types of bipolar disorder. Bipolar 2 disorder involves periods of hypomania and depression. As soon as a person has a full manic episode, they no longer meet the criteria for bipolar 2. From that point on, bipolar 1 disorder will be the most accurate diagnosis.
So it’s possible for someone who was originally diagnosed with bipolar 2 to need a new diagnosis if they start having manic episodes. However, the opposite is not true because once you have one manic episode, you can’t go back to having bipolar 2 disorder.
Find care with Rula
Bipolar 1 and bipolar 2 disorder share many similarities, but they are distinct conditions. And the main difference between the two conditions is mania versus hypomania. Fortunately, both types of bipolar disorder are manageable with the right support.
Rula takes the guesswork out of finding the right therapist for you with our therapist-matching program. In less than three minutes, you can match with a therapist who takes your insurance. And our network of over 15,000 therapists means you can be seen as soon as tomorrow — from the comfort of your own home. And if medication is a part of your treatment plan, we can also connect you with an in-network psychiatric provider.